MTSU’s Center for Health and Human Services supports better health and well-being for all — and that includes healthy sleep, which is why CHHS is sharing useful information this week in observance of Sleep Awareness Week and World Sleep Day this Friday, March 19.
The most dangerous sleep disorder is obstructive sleep apnea, or OSA, which untreated has up to a 40% chance of death within 12-15 years.

Dr. William Noah

Cynthia Chafin
Dr. William H. Noah, senior medical director for Sleep Centers of Middle Tennessee, has been practicing sleep medicine for more than 25 years and also serves as chairperson of the MTSU Sleep Research Consortium. He and Consortium Director Cynthia Chafin, CHHS associate director with two decades of public health experience, put together some helpful information about OSA.
Here’s what they had to say:
Untreated high blood pressure, also called hypertension, may be less deadly than OSA. High blood pressure, or HBP, is known as the “silent killer” because it often goes unnoticed until it is too late. If HBP is the “silent killer,” then OSA is the “loud killer” — loud because most patients with OSA snore.

Middle Tennessee State University’s Center for Health and Human Services has formed a research partnership to highlight the importance of sleep quality in the overall health of Tennesseans and that of the nation. (Photo by Ketut Subiyanto from Pexels)
The “loud killer” causes “silent killer.”
Research shows that 60%-83% of patients with high blood pressure have OSA. The “loud killer” is actually a major cause of the “silent killer.” The body triggers the “fight or flight” reaction to relieve the obstruction (snoring), which in turn raises blood pressure. All patients with hypertension who snore should be tested for OSA.
The “loud killer” causes Type 2 diabetes.
Up to 86% of patients with Type 2 diabetes have obstructive sleep apnea. The “fight or flight reaction” raises blood sugar and insulin levels. All patients with Type 2 diabetes should be tested for OSA.
The “loud killer” causes heart disease.
Roughly 60%-82% of patients with heart disease have OSA. All patients with heart disease who snore should be tested for OSA.
Despite being “loud,” most snoring is Ignored and most OSA goes undiagnosed.
Roughly 2 in 3 adult Americans have OSA, more than hypertension. OSA is three times more common than Type 2 diabetes. While screening for HBP, cholesterol, and Type 2 diabetes are standard in a medical practice, testing for OSA is uncommon.
The “loud killer” needs a new name.
The word “apnea” is misleading. Many patients with OSA do not have apnea. The name “OSA” causes many to think they must “stop breathing” or “hold their breath” in their sleep. They do not realize that snoring alone is reason to seek evaluation.
Treating OSA is now simple and fast.
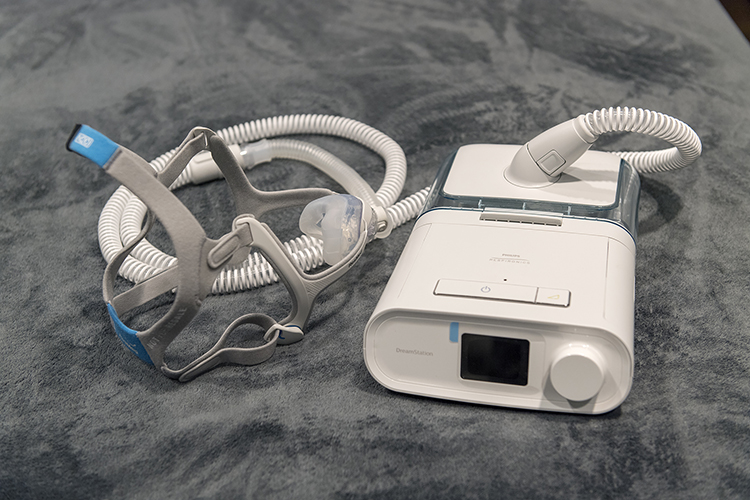
This machine used to administer continuous positive airway pressure, also known as CPAP, is like those used as the Sleep Centers of Middle Tennessee to treat those suffering from sleep apnea. The Sleep Centers of Middle Tennessee has partnered with the MTSU Center for Health and Human Services to form a consortium conducting sleep research. (MTSU photo by Andy Heidt)
Anyone experiencing problems with sleep is encouraged to find a sleep medicine clinician that he or she feels comfortable with to get an assessment.
Wearing CPAP is no longer a problem.
In January 2021, the Journal of Clinical Sleep Medicine published data from over 4,000 Sleep Centers of Middle Tennessee patients showing those provided CPAP — or continuous positive airway pressure — devices by Sleep Centers were 50% more likely to wear their CPAP long term than if CPAP was provided by a medical equipment company.
It is up to you to increase awareness.
This week, we challenge you to listen for the “loud killer” among your family and friends. Ask your bed partner if you snore. Warn them that snoring is a dangerous sound.
About the MTSU Center for Health and Human Services
The Center for Health and Human Services seeks to improve the health and well-being of Tennesseans. The Center, in partnership with the Adams Chair of Excellence in Health Care Services, initiates and strengthens academic programs in health and human services to support workforce development and promote healthy communities. For more information or to learn how the center can help meet your organization’s research, training, or education needs, contact Cynthia Chafin at 615-898-5493 or Cynthia.Chafin@mtsu.edu or visit the center’s website at http://www.mtsu.edu/chhs/.


COMMENTS ARE OFF THIS POST