by Allison Gorman
In 2021, Leeanne Harris gave birth to a boy and gave him away. If he couldn’t go home with her, she thought, he could at least go home with his big brothers, ages 2 and 5. They’d been adopted by a family friend.
“That’s the major thing—I had to sign custody over of my oldest two,” Harris said. “When I had my third, I also gave him up, because I wanted them all together. I didn’t want them to be separated.”
Harris, who lives in Lebanon, lost custody of her three children because she’d lost battle after battle against meth and heroin. She’d tried rehab, including medication-assisted treatment (MAT) with suboxone, several times without success.
That’s the way addiction often looks, said Dr. Josh Wienczkowski, because addiction is a chronic disease. Wienczkowski is medical director at Lebanon-based Cedar Recovery, where Harris had tried and failed to get clean with MAT.
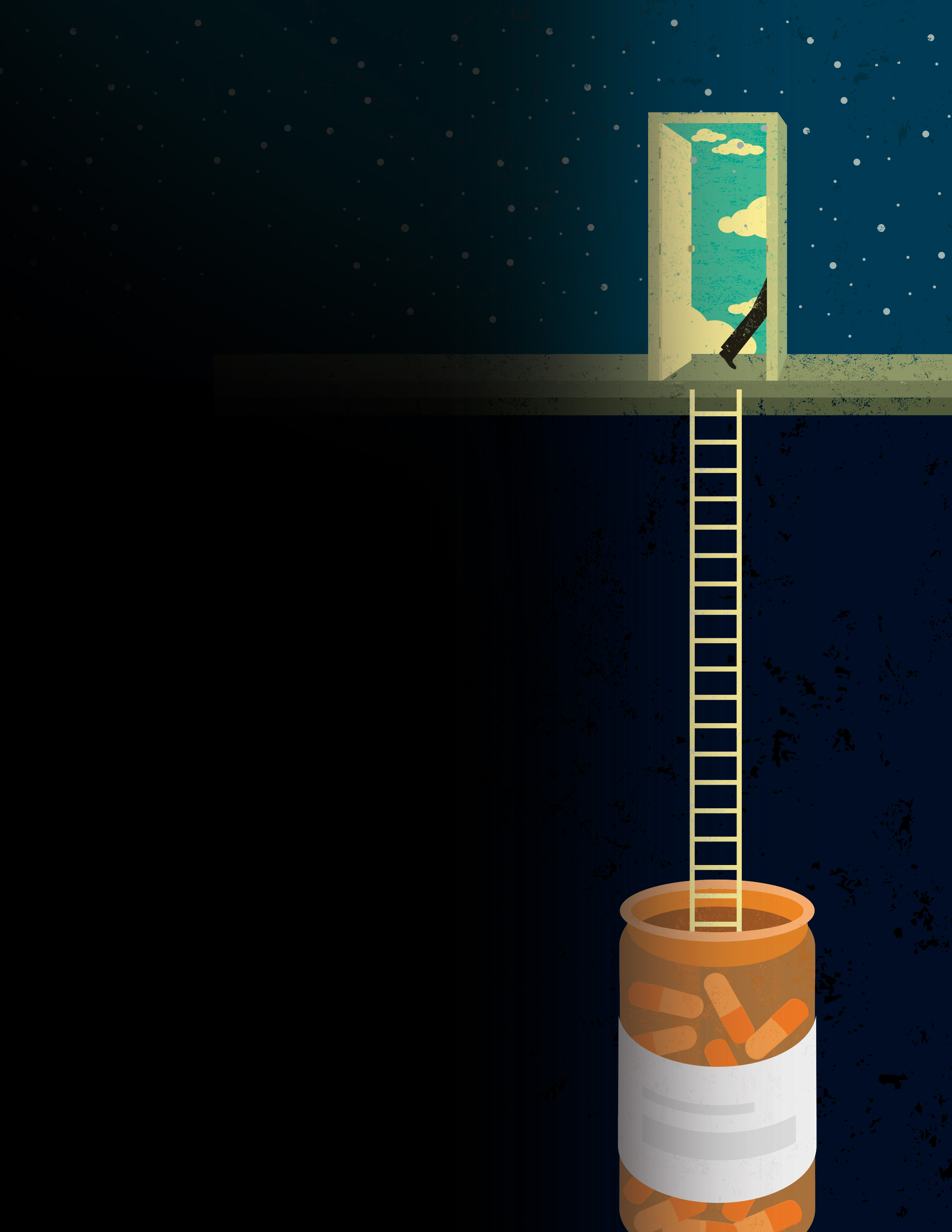
Just like cancer, diabetes, or high blood pressure, substance use disorder (SUD) is characterized by periods of relapse and remission. It’s unrealistic to expect full recovery after a single course of treatment, Wienczkowski said. And with SUD, as with other chronic diseases, recovery can be complicated by depression, financial hardship, or any number of internal or external stressors. The important thing is to keep trying.
“What’s comforting is that current literature shows the vast majority of those with SUD will recover fully—over 70%,” he said. “And time in both treatment and recovery only increases that number.”

Harris can’t recall exactly how many times she tried MAT, and she’s not sure what made the last time different. All she knows is she was desperate to see her kids, including her baby, so she tried it again, and it stuck.
Over the next year, she got clean, got a job, got a car. Then she lost TennCare, her government health insurance. It had been paying for her medication and counseling at Cedar.
The forward momentum stopped.
“I wanted to be in my kids’ lives,” Harris said. “I wanted to watch them grow. But it seems like when one little bump comes up, and you’re in recovery, you want to give up.”
That’s where she was—about to give up—when she got the call from Wienczkowski. Thanks to MTSU and a volunteer group, DrugFree WilCo, he had grant funding to continue her treatment.
A STATE IN PERIL
Harris is convinced that the grant saved her life. Given how lethal opioid overdose is (see sidebar below), that could very well be true.
The opioid epidemic has hit Tennessee hard. The U.S. Centers for Disease Control and Prevention ranks the state second for the rate of opioid prescriptions dispensed per 100 persons. For people susceptible to SUD, an opioid prescription can lead to fatal addiction. Between 2011 and 2021, according to the Kaiser Family Foundation, opioid overdose deaths increased by 240% in the nation overall and 350% in Tennessee. In 2021 alone, there were 63 opioid-related deaths in Wilson County, where Harris lives.
I WANTED TO BE IN MY KIDS’ LIVES. I WANTED TO WATCH THEM GROW.

The Rural Communities Opioid Response Program (RCORP) grant from the Health Resources Services Administration offers a lifeline for people like Harris, who face financial or logistical barriers to MAT. Paul Trivette, chief strategy officer at Cedar Recovery, said even if someone can’t afford inpatient rehab— the ideal first step for treatment—the grant provides continued access to suboxone, which controls opioid cravings but is extremely expensive. Having that medication can keep people from sinking until they learn how to swim.
As Trivette put it, “You can’t treat dead people.”It was the death of Thomas Tapley, a young Wilson County resident who appeared to have beaten addiction, that inspired the founding of MTSU’s grant partner, DrugFree WilCo. Tapley overdosed days before he was set to play a leading role in The Piano Lesson at Lebanon’s CenterStage Community Theatre.
When Tapley’s mother asked Wilson County Mayor Randall Hutto to do more to address the opioid crisis locally, Hutto assembled a team of civic leaders to explore solutions. One of them was Michael Ayalon—then president of Lebanon’s Rotary Club, and now a doctoral student at MTSU.
The solution they came up with was an innovative collaboration of 12 community sectors from Wilson County, including schools, businesses, faith-based organizations, the health care system, and courts and law enforcement.
THE OPIOID EPIDEMIC HAS HIT TENNESSEE HARD.
DrugFree WilCo tackled the crisis from several angles. With an initial Comprehensive Opioid Abuse Program grant of $532,000, they placed a reentry transition specialist inside the Wilson County Jail, to give inmates with SUD a better chance of staying clean after incarceration. They established the Preventing Incarceration in Communities (PIC) Center, a prison-diversion program designed to decrease crime, reduce recidivism, and combat addiction. They raised public awareness about SUD through educational programs at businesses and schools. They distributed naloxone, the nasal spray that can reverse a potentially fatal overdose.

It was a lot, Ayalon said, but it wasn’t enough. If they were going to solve the opioid crisis in Wilson County, they needed more funds.
So he teamed up with Cindy Chafin, director of MTSU’s Center for Health and Human Services. Chafin secured two RCORP grants—an initial $200,000 for 18 months of planning and then $1 million for three years of implementation—to break down more barriers to MAT, from lack of insurance to lack of transportation to treatment. Ayalon assumed the role of Wilson County RCORP coordinator, the liaison between MTSU and DrugFree WilCo.
The RCORP grant is what kept Leeanne Harris from giving up and going under. At press time, she was well on her way toward two years clean and sober.
BATTLING MISCONCEPTIONS
Some barriers to treatment begin as misconceptions. MTSU and DrugFree WilCo are taking those on too.
Viewing addiction as a moral failure rather than a chronic disease can prevent people with SUD from seeking treatment. It can also prevent government investment in effective solutions. So, part of the RCORP grant has gone toward education, Ayalon said. It’s paid for a countywide billboard campaign promoting treatment and recovery. It’s funded MAT training for the county’s law enforcement officers.
It’s paid for annual assessments of the effectiveness of DrugFree WilCo’s efforts to destigmatize SUD.
They’re making a measurable difference, Ayalon said. But there’s more work to be done.
“I think there’s still some hesitation and concerns with medication-assisted treatment that need to be answered for the community,” he said.
He hopes to alleviate those concerns by offering educational programs at churches and hosting lunch ’n’ learns with community leaders.
One thing that’s hard to quibble with is the cost-effectiveness of preventing and treating SUD. “Investment of time, energy, resources, and money into substance use disorder treatment has one of the highest return rates to society of all diseases,” Wienczkowski said.

Every dollar spent on SUD treatment saves $4 in future health care costs and $7 in criminal justice costs, he said. Every dollar spent on evidencebased interventions—as opposed to “just say no” programs—saves up to $58 in future costs.
Then there’s the incalculable return on investment: lives saved, relationships repaired, families salvaged, trauma averted.
“Investing in substance use disorder treatment means not only helping an individual return to a fully functional member of society; it means generational change where we impact their entire family, support system, and community,” Wienczkowski said.
That can be a hard sell in a country that has historically treated addiction with ostracization and punishment, despite lack of results.
“If incarceration cured substance use disorder, the U.S. would be leading the world in recovery outcomes, not overdose deaths,” Wienczkowski said.
EVERY DOLLAR SPENT ON EVIDENCE-BASED INTERVENTIONS SAVES UP TO $58 IN FUTURE COSTS.
SEEING ADDICTION DIFFERENTLY
As program director of the PIC Center in Wilson County, , Derrell Seigler has witnessed the transformative power of effective SUD treatment. Since he founded the center in 2021, it’s had 50 graduates—50 successes measured by six-month treatment program completed and prison sentence averted. Every one revealed the human promise behind the disease.
“I have testimonies of people saying how it changed their lives,” Seigler said. “They’ll go to court and the judge will say, ‘You look completely different.’ A lot of these clients have even had their fees and court costs dropped. Everything’s been covered. To me that’s where the recidivism comes in. When someone doesn’t feel like they have support or have somewhere to go . . . they’re going to go back to what they know.”
He recalled one woman who came to the PIC Center having failed three different treatment programs. Seigler found a program that worked for her, and she turned her life around, eventually reuniting with her adult daughter.
Most people don’t see that side of the addiction story, he said. They just see the addict and think, She’s always been that way. And she’s probably going to die in jail
Trivette understands that narrow view as well as anyone.
TWO WEEKS BEFORE HE DIED,” TRIVETTE SAID, “MY FATHER LEFT ME A VOICEMAIL THAT I STILL HAVE TO THIS DAY.

Before he became an addiction-treatment professional, he was a registered lobbyist. His job was to convince lawmakers that addiction is a chronic disease and that MAT is worthy of public investment.
Before he was a lobbyist, he was a police officer in Bristol, Tennessee. Law enforcement works on the front lines of the opioid crisis. Trivette’s first day as a cop, he got a call from the Los Angeles Police Department. His dad had died of an overdose.
Trivette’s dad had already served time in Tennessee for stealing from Paul and Paul’s mom. He’d fled to L.A. to avoid arrest after breaking into his brother’s house.
“Two weeks before he died,” Trivette said, “my father left me a voicemail that I still have to this day, telling me that he was sorry, that he loved me. I refused to call him back. I wish I hadn’t.”
It took nearly five years for Trivette to think about his dad, and addiction, in a new light. The change began when Matthew Hill, a state legislator at the time, asked him to work as an advocate for people with SUD.
Trivette initially declined, saying he didn’t accept the premise that addiction was a disease.
“I know what it’s like,” he said. “I see what it’s like on the streets.”
Hill pushed back, acknowledging that he once felt the same way. He invited Trivette to attend a discussion of SUD by clinical professionals, including Dr. Loyd Stephen, chief medical officer of Cedar Recovery.
Learning how opioid addiction rewires the brain was powerful medicine for Trivette. For the first time, he understood what his father had been up against.
“That’s why I want to be part of the change now,” he said. “To help other families and other people that have been impacted by addiction maybe have another mindset, maybe not stigmatize their loved one that’s battling an unbelievably powerful illness—so much so that the very thing that your brain desires will be the thing that kills you.”

THE BOTTOM LINE
Keeping people alive. For DrugFree WilCo, that’s the bottom line, and they’re always pursuing new strategies to do it.
At the top of Ayalon’s wish list is ODMap, a webbased tool that tracks overdoses in real time. A cluster would indicate the presence of a particularly lethal batch of drugs.
“If suddenly we see three or four overdoses on the same block, that tells us there’s a problem in that particular community,” he said. “So we would dispatch a mobile unit to that area fully stocked with naloxone and fentanyl test strips.”
More help is already on the way to help others battle opioids, thanks to new grants awarded to CHHS. Another $2.92 million RCORP federal grant, awarded to the center in partnership with Cedar Recovery, will establish the first mobile unit providing MAT in Tennessee with access points in five rural counties—Giles, Hickman, Franklin, Lawrence, Marshall—plus a brick-and-mortar location in a sixth rural county, Claiborne.
The MTSU center also recently received $9.1 million from Tennessee’s Opioid Abatement Council in community grants funded by legal settlements with opioid producers, distributors, pharmacies, and marketers. This will help fund aftercare services and six respite centers across Tennessee providing housing to those waiting on beds in treatment facilities.
Ultimately the goal is to buy time. To give struggling people one more try at living.
I DON’T GET TO TAKE THE BOYS AND LEAVE WITH THEM,” HARRIS SAID, “BUT I CAN VISIT THEM, SPEND TIME WITH THEM, GO WHEREVER THEY GO.
Leeanne Harris got another try at motherhood, albeit on new terms.
“I don’t get to take the boys and leave with them,” she said, “but I can visit them, spend time with them, go wherever they go.”
Last Halloween when they went trick or treating, she went with them.
One more try, one more day, one more moment. “It was amazing,” she said.
A Complex Enemy
Opioids, a class of drugs naturally derived from the opium plant, include prescription medications like hydrocodone, oxycodone, codeine, and morphine; the illegal drug heroin; and synthetic medications like fentanyl.
It’s not uncommon for someone with substance use disorder (SUD) to become addicted after being prescribed opioids for pain relief, and then turn to street drugs when their legal access dries up.
What makes opioid addiction uniquely dangerous is the high risk of death from a single use, said Paul Trivette, chief strategy officer of Cedar Recovery in Lebanon.
Most drug-related deaths result from the physiological damage caused by prolonged, heavy use, he said. It’s rare for someone to die overnight from drinking alcohol, for example, or from ingesting stimulants like cocaine or methamphetamines. But one overdose of opioids can cause potentially fatal respiratory depression. And for an opioid addict, the cravings are physically overwhelming.
“If someone is using heroin and they quit cold turkey, or if they go without it for some period of time . . . the brain signals to them, You need more opioids so you don’t die,” Trivette said.
The presence of fentanyl in meth and other street drugs has ratcheted up the danger level, he added. While fentanyl is used medically at microgram strength as anesthesia, it’s used illegally at milligram strength, which is a thousand times more powerful.
“That’s why opioids are such a difficult battle for people,” he said. “Because of the high rate of death, the withdrawal symptoms that it causes, and the fact that you think that you’re taking a certain amount of the opioid, and you’re actually taking a lethal dose and you don’t wake up again.”
Breaking Barriers
The Rural Communities Opioid Response Program (RCORP), which awarded $1.2 million in grant funding to MTSU and DrugFree WilCo, is one of several government initiatives addressing the opioid crisis. As a result, it’s getting a little easier to help uninsured people pay for suboxone, the expensive medication that suppresses the intense symptoms of opioid withdrawal, said Paul Trivette, chief strategy officer at Cedar Recovery in Lebanon. A bigger barrier to treatment now is lack of transportation.
DrugFree WilCo is using the RCORP grant to take on that problem too.

Cindy Chafin, director of MTSU’s Center for Health and Human Services
When patients don’t have to worry about how they’ll get their medication, Trivette said, “we can help them focus on getting a job if they need one, getting their children back if they’ve lost their children, maybe building relationships back with their family and friends that they lost, maybe food insecurity. We can start addressing those things because now their mind is not so focused on not being dopesick.”
One of the main reasons people fail to follow through with medication-assisted treatment is that they can’t get where they need to go to receive it, he said.
That’s an especially common problem for clients at the Preventing Incarceration in Communities (PIC) Center, established by DrugFree WilCo at Cedar Recovery as a prison-diversion program for first-time drug offenders. Often people who’ve been ordered to receive treatment don’t have a driver’s license or reliable transportation.
The Wilson County-based PIC Center partnered with Uber Health to get people to their court-ordered appointments. It also uses donated funds to buy bus passes or subsidize personal transportation.
Derrell Seigler, program director at the PIC Center, said they’ve helped about a fifth of their clients get to treatment this way. The most expensive trip was a $118 Uber ride to downtown Nashville.
Not much for a ticket to life and freedom.

COMMENTS ARE OFF THIS POST